Common Questions Asked By Families
OCNDS was first identified in 2016. Due to its recent discovery, there is still much we don't know about this syndrome. This can be incredibly frustrating, particularly after receiving a life-altering diagnosis. We are making significant strides in understanding OCNDS thanks to the participation of our community in the Simons Searchlight Natural History Study and Ciitizen; however, to gain more insight, we need more participation from each and every family. As we gather more data and insights, we hope to provide answers to the many questions parents of children with OCNDS may have. See Family Research Opportunities to see how you can participate.
Every OCNDS parent is an expert in how this syndrome presents in their child, and sharing experiences and knowledge within our supportive community can be invaluable. We encourage caregivers to join our closed
Facebook group, where caregivers can connect with other parents facing similar challenges. Together, we can navigate the uncertainties of OCNDS and work towards a brighter future for our children.
DISCLAIMER
The information provided is for general informational purposes only and is not intended as, nor should it be considered a substitute for, professional medical advice.
Where indicated, “Parent response” denotes that a parent of a child with OCNDS provided this response and it does not necessarily represent the views of the foundation.
DIAGNOSIS
Are there any parents who found out that they have OCNDS after searching for their child’s diagnosis?
Yes, we have some families who passed down the mutation, and they also learned about their diagnosis because their child was diagnosed. There was a publication describing examples of this in 2023. You can see the research explained here.
What does it mean if my child’s genetic report says the DNA change is a ‘variant of uncertain significance’?
Variants in the DNA change the instructions for making proteins. Pathogenic variants change important instructions in your DNA and are “disease-causing.”
- When a variant has uncertain significance, it means that scientists don’t have enough information to decide if the variant causes disease or not. Scientists use many different pieces of information, like pieces of a puzzle, to decide if a variant is pathogenic. Missing pieces mean you can’t finish the puzzle and see the full picture. When scientists lack information, they are uncertain if a variant is pathogenic.
- You can learn more about how to read your genetic report via this informational video.
- Learn more about Variants of Uncertain Significance from Genetic Counseling Masters' Student Intern, Grace Snyder, via this handout or watch this video.
Is there a central database where everyone with OCNDS is registered?
We ask all families to register with the foundation here: Contact Registry
How do I talk to my child about having OCNDS?
This is a big conversation, and there’s no one-size-fits-all approach—but honesty, reassurance, and age-appropriate explanations are great places to start.
While we don’t yet have our own book specific to OCNDS, we highly recommend Chromosome Kids Like Me by Annette Fournier. This beautifully written book uses a fun and simple analogy—socks!—to help kids understand chromosome disorders in a way that makes sense to them. Written by a fellow rare disease parent and reviewed by a geneticist, it’s a great tool for starting the conversation about what makes each of us unique. Check it out here.
DOCTOR APPOINTMENTS
What should we ask our doctors?
We have a guideline published as a Gene Review. You can print it out and take it to your doctors, and they will see the guidelines and recommendations on what to do by each specialty.
What are some of the things that we should be testing for? Is there a list of potential issues that come with OCNDS that we should be on the lookout for specifically and testing for?
For care recommendations, please see a simplified version of the Gene Review publication authored by Dr. Okur and Dr. Chung: OCNDS GeneReviews Overview
Dr. Chung talks about several things in this lecture.
Do you have a list of doctors who see OCNDS patients?
We have started to collect information from families about their doctors. If you have a doctor you recommend, please submit their information here.
INSURANCE
What is the OCNDS ICD-10 code for insurance?
There is no specific ICD-10 code for OCNDS yet. It is an active goal of the foundation. We are applying for approval at the Fall 2024 meeting.
For insurance purposes, many people use Apraxia codes, developmental delay, and autism (if there is a diagnosis). For some families, the genetic diagnosis led to the utilization of code Q 99.9 “genetic defect” as a generic code. Prior to the OCNDS diagnosis, they just utilized other diagnosis- intellectual disability, stereotypy, etc.
OCNDS SYMPTOMS
What symptoms are most impactful on those with OCNDS?
Per a Simons Searchlight Survey in 2022, the symptoms with the greatest impact are:
- Intellectual disability/delay
- Limited or absent speech
- Sleep
What are all of the reported symptoms in OCNDS?
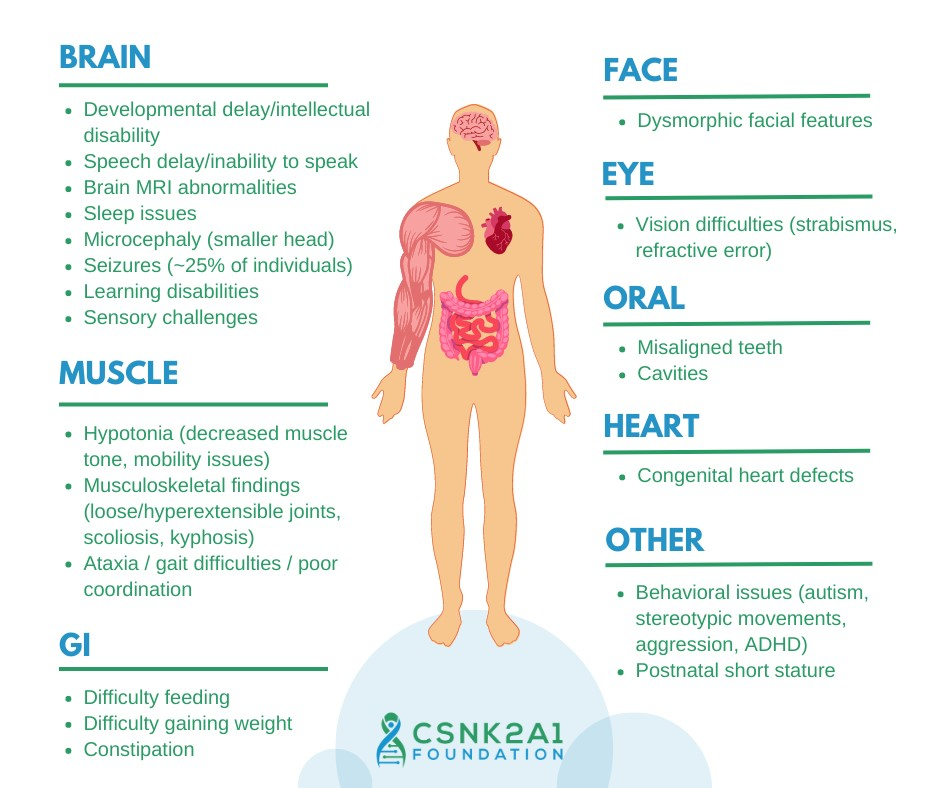
This graphic highlights known OCNDS symptoms.
Symptoms of OCNDS Text Version
Brain
- Developmental delay/intellectual disability
- Speech delay/inability to speak
- Brain MRI abnormalities
- Sleep issues
- Microcephaly (smaller head)
- Seizures (~25% of individuals)
- Learning disabilities
- Sensory challenges
Muscle
- Hypotonia (decreased muscle tone, mobility issues)
- Musculoskeletal findings (loose/hyperextensible joints, scoliosis, kyphosis)
- Ataxia / gait difficulties / poor coordination
GI
- Difficulty Feeding
- Difficulty gaining weight
- Constipation
Face
- Dysmorphic facial features
Eye
- Vision difficulties (strabismus, refractive error)
Oral
- Misaligned teeth
- Cavities
Heart
- Congenital heart defects
Other
- Behavioral issues (autism, stereotypic movements, aggression, ADHD)
- Postnatal short stature
Is there any explanation why the syndrome is more severe in some people, with more comorbidities?
Some studies suggest that specific gene changes may yield distinct symptom profiles and/or severity levels. For example, see the research explained here. Additional studies are ongoing to investigate if changes in different parts of the gene cause specific symptom profiles.
Do certain variants of the CSNK2A1 gene create different symptoms?
The symptoms range from mild to severe regardless of the variant. Every child is unique in how the syndrome presents. There is some data to suggest that individuals with DNA changes that cause the protein not to be made may have a milder symptom profile than individuals who have missense mutations (where only one building block of the protein is replaced because of the mutation and the protein continues to be produced although its function is altered). You can learn more about this study by reading this research explained.
Seizures/Neurological
Is there a particular medication used to treat seizures with OCNDS?
According to reports in the Simons Searchlight natural history study, Levetiracetam and Phenobarbital stood out as particularly effective for OCNDS patients.
Does everyone with OCNDS develop seizures?
Not everyone with OCNDS will develop seizures. Current estimates are between 25-33% of individuals with OCNDS that will develop seizures. As of April 2024, based on 23 individuals registered in Simons Searchlight natural history study, the age of seizure onset varied from 2 months to 16 years, with an average age of first seizure at 3.1 years, demonstrating wide variability across patients. As of April 2024, the most commonly reported seizure types are Petit mal and Grand mal seizures.
Are headaches a symptom of OCNDS?
Headaches can be an underlying symptom of seizures.
Gastrointestinal
My child has been vomiting at night for no apparent reason. Is this a symptom of OCNDS?
Currently, the foundation does not have data to show that this is a symptom.
Parent response: For my child, these episodes were generally related to mucous draining (due to infection or just viral infection) or increased reflux. Once we had reflux more under control & less illness it got much better. She still has issues at times but has improved since she was younger.
She has also had issues with random vomiting which we linked to exposure to chlorine/pool chemicals in various pools irritating her asthma when she was younger.
Are stomach pain and constipation symptoms of OCNDS?
Constipation is a common symptom reported in OCNDS. Approximately 63% of families in the Simons Searchlight natural history study report gastrointestinal issues.
Musculoskeletal
My daughter breaks her bones easily. Is this a symptom of OCNDS?
Approximately 15% of OCNDS families in the Simons Searchlight natural history study report orthopedic issues (relating to the branch of medicine dealing with the correction of deformities of bones or muscles), including scoliosis (a spinal deformity that causes the spine to curve to the side, forming a C or S shape).
Is hip/joint pain a symptom of OCNDS?
Approximately 10% of OCNDS families in the Simons Searchlight natural history study report joint problems.
Parent response: Our almost 11-year-old has what the Drs call crouch walk. She just got fitted with orthotics. She doesn’t talk much but I know her knees are hurting her because she keeps sitting down when walking.
Vision
Could vision problems that are unrelated to the parents be due to the syndrome?
Vision problems are common in patients with OCNDS and across neurodevelopmental syndromes. According to April 2024 updates from the Simons Searchlight natural history study, 37% of individuals with OCNDS experience astigmatism and 21% have crossed eyes.
Speech
Is speech delay a symptom of OCNDS?
Yes, speech delay is the most significant symptom of this syndrome and is considered a hallmark symptom of OCNDS. According to April 2024 updates from the Simons Searchlight natural history study, almost all (99%) of individuals with OCNDS have some level of language delay/impairment. The recommendation is to start speech therapy as early as possible. But it's never too late. It is also recommended to try other methods to develop a vocabulary. Try using communication technologies like an iPad, or other communication tools.
Sleep
My child won’t sleep. How do I help my child to sleep?
Data from the Simons Searchlight natural history study found that the top sleep problems in OCNDS are needing a parent in the room to sleep, restlessness/moving a lot, trouble sleeping away from the home, and not falling asleep within 20 minutes.
Families have reported using a variety of different interventions, including medications (melatonin, clonidine, hydroxyzine), other tools such as a weighted blanket, and methods such as co-sleeping. Some families found benefits by using a tent over the child’s bed for sensory blocking. Other families report using a therapeutic listening program through their occupational therapist. Other families who have children with OCNDS that have seizures noticed sleep improvements once seizure medications were started.
Mental Health
Do individuals with OCNDS struggle with mental health issues (depression, self-injury, anxiety, etc.)? How do we help our child with these struggles?
Yes. According to the April 2024 Simons Searchlight natural history study report, approximately 15% of individuals with OCNDS suffer from anxiety. Top behavioral concerns were impatience (ages 1.5-5 years) and obsessions (age 6-18 years). We have heard from families experiencing issues with self-injurious behaviors.
A new symptom diagnosed in individuals with OCNDS and autism is catatonia. Catatonia in autism is a complex condition marked by changes in movement, speech, and behavior. Symptoms include slowed speech, difficulty initiating tasks, freezing in place, unusual posturing, repetitive movements, and a decline in daily functioning. Some individuals may also exhibit self-injury or aggression, often triggered by frustration or difficulty responding to their environment. These symptoms can be mistaken for regression, leading to delays in recognition and treatment. Early intervention with behavioral strategies, medication, or electroconvulsive therapy (ECT) in severe cases can improve outcomes, making awareness and timely support crucial. To learn more about catatonia, you can watch this video by Dr. Josh Smith at Vanderbilt University.
Parent response: What helped our situation was having an evaluation for depression and anxiety. Medication and therapy have helped. Finding other ways to cope instead of cutting is an ongoing process. This may sound silly, but we made a sensory box that has all things sensory in it, small treats, nail polish, face masks, small art projects etc. that we are constantly replenishing so when our daughter feels overwhelmed, she can use the box items to prevent cutting. It gives us something in the moment to direct her to and help her choose a different way to cope with overwhelming feelings. Visit Crisis Text Line for more information.
My child grinds his teeth because of anxiety. How can I help him?
We don’t have any specific study for this but we suggest contacting your child’s dentist as they may be ablet to help via use of a mouthpiece for the evenings. Another option would be to see a child psychiatrist to discuss anxiety management options.
Short Stature
Do you recommend using growth hormones for someone with short stature and OCNDS?
The information provided is for general informational purposes only and is not intended as, nor should it be considered a substitute for, professional medical advice. We do not have any formal growth hormone studies that are ongoing, but we have heard of other children who have tried this therapy. This decision is between you and your endocrinologist. It might cause reaching the final adult height early, but on the other hand, it could help kids to grow who otherwise would have stunted growth. There are no known OCNDS-specific risks other than the general risks, and the benefits are the same as in any other growth hormone therapy when there is no growth hormone deficiency. We need to collect more information on this. For more information, you can view Dr. Chung’s presentation on growth hormone here. Please visit our research opportunities page to learn more.
LABS
We just got our immunodeficiency panel back and my child has values that are at the low end of normal range. Anyone else have a similar situation?
Based on data in the Simons Searchlight natural history study, approximately 7% of individuals with OCNDS report immunodeficiency. Families have reported low values. Additionally, some families report getting IVIG (intravenous immunoglobulin) therapy with huge improvements.
Are raised inflammatory markers a symptom of OCNDS?
We do not have enough data yet to determine if increased inflammatory markers are a symptom of OCNDS. We are aware that a subset of individuals with OCNDS experience immunodeficiency.
MILESTONES
When are delays noticed?
Most children with OCNDS begin missing milestones and are delayed in reaching milestones. Many have observed low muscle tone, feeding difficulties, breastfeeding difficulties, delayed motor skills such as crawling, pulling up and walking, and speech delay.
What learning milestones have other children with OCNDS achieved and at what age(s)? How can I improve my child’s cognitive and language skills?
Data in the Simons Searchlight natural history study using data from 41 individuals with OCNDS highlights developmental changes using information from a standardized measure called the Vineland Adaptive Behavior Scales (Vineland-3). Some findings were:
- 89% of individuals with OCNDS are likely to be using language at age 4 or older.
- 83% of individuals with OCNDS are likely to be feeding themselves at age 4 or older.
- 74% of individuals with OCNDS are likely to be making eye contact at age 4 or older.
See this summary for more details: Simons Searchlight Registry Update CSNK2A1 (OCNDS)
TOILETING
What advice do you have for toileting issues?
Parent response: Recommended underpants for not quite potty-trained kids (rare, small accidents): Max Shape (can purchase on Amazon). Maybe period underwear depending on size needed.
Parent response: There is a nose spray you can get. My daughter used it for years and helps the brain to detect that she needs to pee. You do 2 sprays one in each nostril and worked like a charm.
Parent response: Desmopressin link (DDAVP) is often the first choice of medicine for bedwetting. This medicine slows the amount of urine your child's body makes overnight, so the bladder doesn't overfill and leak. Desmopressin can work well, but bedwetting often returns when a child stops taking the medicine.
FUTURE PLANNING & EXPECTATIONS
Helpful Videos
Are individuals with OCNDS at higher risk to develop disorders like Alzheimer's, Parkinson's, bipolar disorder, and Neuropsychiatric disorders?
Currently, we don't have enough adult individuals with OCNDS to do follow-up studies. It can happen and emerge in individuals with neurodevelopmental syndromes that are caused by other genes. We can’t say there is no risk, but we also cannot say that there is a definite risk.
How old is the oldest person living with OCNDS?
Currently, the oldest individual with OCNDS that we are aware of is 63.
What is the life expectancy for individuals with OCNDS?
We currently do not have enough information to provide an answer to this question. We hope to learn more about this through our natural history study.
Will individuals with OCNDS be able to live independently as an adult?
This will vary depending on the individual. Every individual with OCNDS is different. The foundation knows of individuals living independently and holding jobs while others will require life-long care.
What should I know about state guardianship?
Please visit our website at Guardianship for more information.
My child with OCNDS wants to get her driver’s license. What should I do?
Parent response: There are businesses/organizations that work with the IDD community to help them get a driver's license. They also help when a person should not get a license. Most driver's license bureaus should be able to give you a local contact name.
Parent response: We had our older son take a defensive driving class. Your insurance person might also know of programs.
Parent response: In Australia there are occupational therapists who teach people with ID to drive. To prepare for the test, there might be an audio version of the driver's manual that your child can listen to while looking at it.
Parent response: My daughter took the class & driving test with the other kids and the instructor. I had to come in and read her the written test. She passed the test on the second try.
THERAPIES
Do you recommend seeing a behavioral therapist? What do you do when your child thinks discipline is funny?
Helpful Videos
- Managing Challenging Behaviors
- Recognizing Anxiety Behaviors and Calming Strategies
- Understanding Problem Behaviors in Neurodevelopmental Disorders
- Speed Sharing Discussion About What’s Working for Managing Behaviors
Parent response: My daughter does ABA therapy but we do a lot of ignoring attention-seeking behavior. At home we just go about the routine. School is harder and she tends to not have as many as before, but she gets put in “time out” which gives her the mental break she may need.
Parent response: I understand it can be frustrating when dealing with a non-neurotypical response and nervous system. Looking from our neurotypical perspective it might seem they are “laughing at discipline” but truly they may not cognitively or developmentally even understand the concept of discipline or be able to understand the concept of the discipline being related to their action.
Parent response: I disagree with ABA. It’s not for everyone. Most adult autistics that had ABA have nothing positive to report about their experience. This being said, I validate other parents’ opinions and don’t say that everyone should listen to me. So no meanness or disrespect meant to those that feel otherwise. I choose to listen to the adult autistic and disabled community who have experienced PTSD from behavioral therapies, and the many research studies that show it as ineffective. I have found a lot of value in Dr. Mona Delahooke’s books and approaches which are not focused on compliance vs. noncompliance but rather on the unique differences of Neuroception. Here is a good video that helps reframe the approach to behaviors: Importance of Respecting Individual Differences in the Context of Relationships- Dr. Mona Delahooke
I’ve heard mixed reviews about ABA therapy (Applied Behavior Analysis). What cognitive behavioral therapies do you recommend?
There is a section in the Gene Reviews publication on ABA. Other than that, it’s usually better to be tailored to the individual kids’ needs, which is called an individual education plan. So, wherever the challenge is, the therapist would focus on that. We don't have anything specific that is recommended for neurodevelopmental disorders to be applied for kids with OCNDS.
Excerpt from the Gene Review publication:
ABA therapy is targeted to the individual child's behavioral, social, and adaptive strengths and weaknesses and typically performed one on one with a board-certified behavior analyst.
- Consultation with a developmental pediatrician may be helpful in guiding parents through appropriate behavior management strategies or providing prescription medications, such as medication used to treat attention-deficit/hyperactivity disorder, when necessary.
- Concerns about serious aggressive or destructive behavior can be addressed by a pediatric psychiatrist.
How do I help my child to speak? What alternative communication apps do you recommend?
Please see the following videos that may be helpful:
- Promoting Learning and Communication in Children with Limited Language
- The Role of Augmentative-Alternative Communication (AAC) Systems
Parent response: We use an iPad to help with communication, and we use pictures also to help, and words are still coming out. We haven't given up hope, but my child has been in speech therapy five days a week since she was 18 months old. Don't give up hope. Keep trying.
Parent response: A lot of words with pictures and music, like associating words with the object. And some sign language. And things like directing attention to her mouth so he would watch the lips. Also, we used Baby bumblebee program. Which I HIGHLY recommend.
Parent response: Music therapy is great, and it helped train his brain for speech.
We are considering using sign language with my child. Does anyone have experience with this?
Parent response: We started with basic sign language. Just the basics like drinking, eating, mommy and daddy. I think we need a lot more practice. He asks for a drink by making the drinking sign, but that's about it. I hoped it would be a way for him to communicate with us, but so far, he doesn't really use it. But you could give it a try, there are a lot of free apps that you can get to learn baby sign language.
Parent response: Absolutely do it!
started to learn sign language when he was an infant. It really helped as he had no speech so just to be able to meet his basic needs was important. Parent response: We taught
several signs around age 1 and it helped until he was speaking around age 3. He started speech therapy at 2, and gradually he was able to speak...went through a period where he’d only speak at home (selective mutism), but by age 5 he was fairly well caught up. Parent response: We continued to use signs from a distance even once my daughter could talk. Helped to say when she was having difficulty in busy environments and when trying to interact with other children.... she could say if there was a problem with other children, without having to verbalize it.
Parent response: We’re in the UK and used children’s books about sign language and Mr. Tumble... the NHS also provided a 6-week makaton course... I found Mr. Tumble more useful though!
Parent response: My son did not start speaking till age 8 and sign was the best way for him to get his message across when we could not understand his words. I knew he understood the sign words when I took him to the fabric store at age 3 and he started signing “all done” repeatedly to get my attention. He is 18 now and signing from a distance or signaling to go to the bathroom is great to know.
How many physical therapy (PT) sessions are OCNDS kids doing per week and what does a typical session look like?
Parent response: Our 2 girls have PT every week for an hour each child. Our 9-year-old is very delayed and didn't walk until 5. She now walks but is very unsteady and has balance problems. Their PT does a lot of fun stuff. Trampoline, riding bikes outside, playing ball, walking up and down stairs.
Parent response:
had PT 1 hour per week age 6 weeks-age 10. Plus, he has done equine therapy from age 2 - now (age 18 and is still doing). When he started school, he was doing 1 hour at home and 1 hour at school for those 5 years. Did not start to walk until after age 3. Parent response: PT went from a few times a week to currently one time a week. She has speech and OT 3 times a week now and has had this for a very long time now at 3 times a week. Her speech/language being the most concerning/delayed. PT - her gross motor skills falling not too far behind. We went through early intervention, to the public school and privately for everything. Lots of core strengthening, balancing, and working on everyday skills such as riding a bike (which she still cannot do by herself), balance beam, trampoline, swinging, jump rope, lifting small things, walking backwards etc.
Parent response:
is 3 years old, has physiotherapy 4 times a week, once a week riding therapy, TO and Speech Therapy once a week and has been swimming for 18 months 2 times a week. He has been walking around since he was 2 years old but has an imbalance. Parent response: We're in the UK and our daughter received a multi-disciplinary approach - saw the physio, SLT and OT at the same time once every 3-6 months from the age of ~2. This continued until she started school at age 5. She eventually walked with a Walker (that we requested) and walked independently about age 4.5.
Besides the most common therapies like physical therapy, speech therapy, and occupational therapy, are there any other therapies that you suggest?
Parents have found the following therapies to be helpful.
- Applied Behavior Analysis Therapy (ABA)
- Speech/Language Pathology / Speech Therapy
- Occupational Therapy
- Physical Therapy / Physiotherapy
- Early Intervention
- Early Intensive Behavioral Intervention
- Behavioral Therapy
- Music Therapy: When the children sing, allegedly it's different than the actual speech region mechanism. They can sometimes sing better than they can talk, and they can learn. And they can show you what they know, their ABCs and one, two, three, and they can also follow as they are learning, maybe to play an instrument or sing a song. You can watch a video about music therapy here.
- Equine Therapy: Those who have had more severe speech problems, or even just motor problems, have used something called equine therapy, which is horse therapy. It helps work on the core. They can also work on speech and following directions and things like that, as they're working on the horse. You can watch a video about equine therapy here.
- Floortime Therapy
- Vision Therapy
- Communication Technology
OCNDS RESEARCH
Is research being done on OCNDS?
Yes. To find out more about how you can participate in ongoing research, please visit https://www.csnk2a1foundation.org/family-research-opportunities
To read summaries of OCNDS research publications, please visit https://www.csnk2a1foundation.org/research-explained
Simons Searchlight
If a family is having trouble signing up, who should they contact?
Simons Searchlight Study Coordinators are always available to help families and participants with questions related to registration. Additionally, the Simons Searchlight team can help answer questions related to genetic lab reports, surveys, blood draws and more. They also address questions in their Facebook groups, but questions in the Facebook groups may not get answered as quickly as a direct email or phone call.
To learn more about why participating in the natural history study is important, please see this video by Dr. Chung. You can also watch a question-and-answer session here.
To learn how to generate a Simons Searchlight Account, please watch this video.
Email: coordinator@simonssearchlight.org
Phone: 1-855-329-5638
