Research Strategy
We are focused on areas that will bring the most value to the OCNDS community as quickly as possible. Thus, our efforts to date have focused on the development of a research toolbox and establishing an experienced scientific advisory board. The full phenotypic range of OCNDS is currently unknown, and major questions regarding disease progression and features in adulthood remain unanswered. Our current efforts are:
Landscape analysis and toolbox expansion
- Determining who is researching CSNK2A1 and related science to engage with them and learn more about the biology of OCNDS.
- Ensuring that the scientific tools we develop for research are accurate and readily available to interested researchers.
- We are actively enrolling individuals in the Simon’s Searchlight Natural History Study. This collects high-quality, standardized data about individuals with OCNDS over their lifetime.
Biomarker development
- Learning more about OCNDS biology to see if there is an OCNDS biological marker (“biomarker”)
- To find a biomarker, we are funding the establishment of mouse models that have DNA changes that have appeared in OCNDS patients and measuring many biological variables including behaviors that are often observed in individuals with autism.
- We are also establishing induced pluripotent stem cell (iPSC) lines. Induced pluripotent stem cells are special because scientists can take regular cells, like skin cells, and use special techniques to turn them back into stem cells. This makes those cells able to do different jobs again, just like they would during early human development. You can think of iPSCs as chameleon cells that can transform into different cell types and help scientists understand and treat diseases better.
Therapeutic testing
- We have not yet funded work towards specific therapeutic testing. Once we have established mice and/or cells with potential biomarker(s), we can explore high-throughput screening techniques to see if there are compounds that can reverse symptoms and/or improve the biomarker(s).
- We plan to fund “proof of concept” studies (i.e., research studies that provide evidence to demonstrate that something is feasible) for gene editing therapeutic approaches (e.g., gene therapy, antisense oligonucleotides (ASOs)).
Infographic
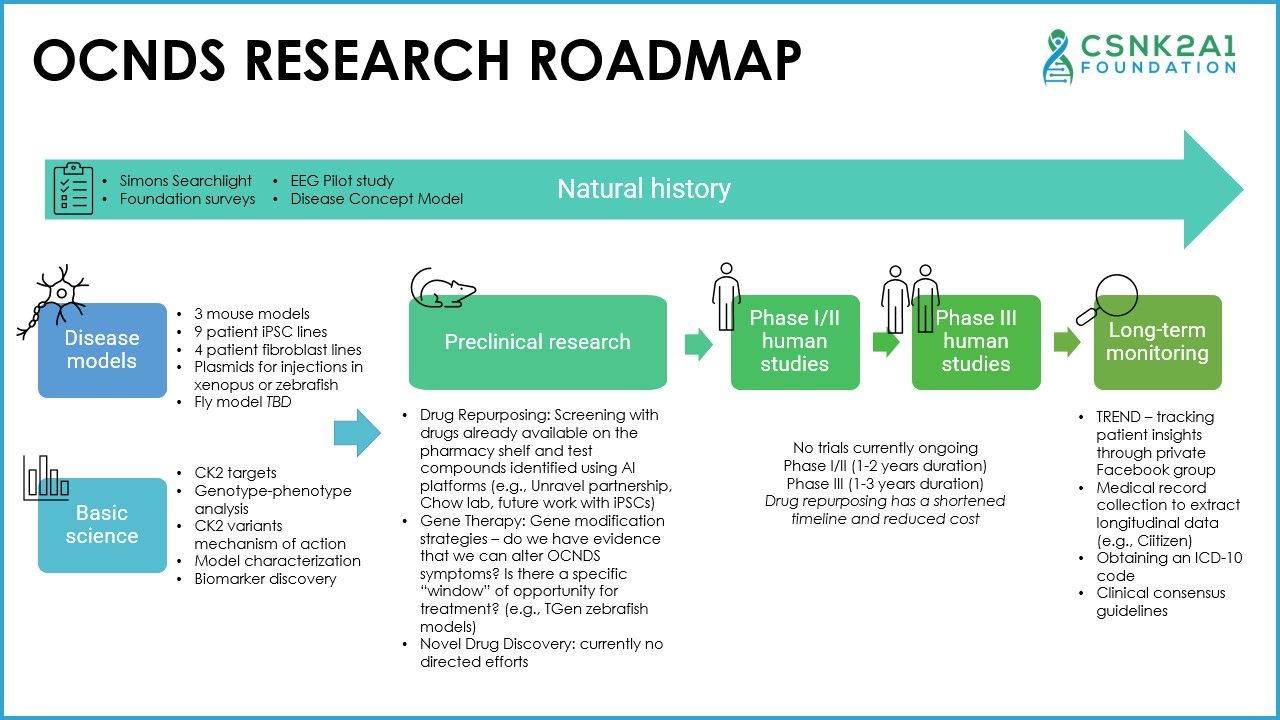
OCNDS Research Roadmap Text Version
Natural history
- Simons Searchlight
- Foundation surveys
- EEG Pilot study
- Disease Concept Model
Disease models
- 3 mouse models
- 9 patient iPSC lines
- 4 patient fibroblast lines
- Plasmids for injections in xenopus or zebrafish
- Fly model TBD
Basic Science
- CK2 targets
- Genotype-phenotype analysis
- CK2 variants mechanism of action
- Model characterization
- Biomarker discovery
Preclinical Research
- Drug Repurposing: Screening with drugs already available on the pharmacy shelf and test compounds identified using AI platforms (e.g., Unravel partnership, Chow lab, future work with iPSCs)
- Gene Therapy: Gene modification strategies – do we have evidence that we can alter OCNDS symptoms? Is there a specific “window” of opportunity for treatment? (e.g., TGen zebrafish models)
- Novel Drug Discovery: currently no directed efforts
Phase I/II human studies and Phase III human studies
No trials currently ongoing
Phase I/II (1-2 years duration)
Phase III (1-3 years duration)
Drug repurposing has a shortened timeline and reduced cost
Long-term monitoring
- TREND – tracking patient insights through private Facebook group
- Medical record collection to extract longitudinal data (e.g., Ciitizen)
- Obtaining an ICD-10 code
- Clinical consensus guidelines
To find treatments for OCNDS, scientists must understand what causes the syndrome and how the body is affected over time. This is a basic roadmap describing the therapeutic development process that we have broken down into 7 steps: disease models, basic science, natural history study, preclinical research, Phase I/II trials, Phase III trials, and long-term monitoring.
Disease models
Are very important to conducting rare disease research. One approach is through animal models. Scientists use non-human animals, such as mice, to learn more about how a disorder may develop or progress in humans. Other tools include repositories for biological samples such as human tissues, blood, cells, or DNA. These samples can be used in studies and for some sample types, create cell lines.
- For example, induced pluripotent stem cells (iPSCs) can be created from skin or blood cells. These cells can be “instructed” in a dish to create cells that are copies of what we would find in the human body. These “models in a dish” are important to understand disease progression and provide a model that can be used to test how cells may react to different treatments.
Basic science research
investigates how a disease works at the molecular, cellular, and organism level and this is a critical step towards finding treatment(s). Understanding how a syndrome affects the body helps researchers identify ways to measure treatment response(s) and discover novel therapeutic strategies.
Natural history studies
collect medical information from individuals over time. They capture longitudinal data to describe how a disease progresses. Data are included from medical records, clinical encounters, and data directly contributed by the patient or caregiver. Importantly, natural history studies may be used to replace the placebo arm in clinical trials when small populations lead to challenges enrolling enough patients.
Preclinical research
focuses on efforts to show that a therapy is safe and effective before introducing it to humans. Both animal research (safety testing) and non-animal research (computer models, cell lines) can be used. Any research focused on a drug or treatment for a disease that occurs before it is tested in human volunteers can be considered preclinical research. The main goals of these studies are to determine a safe starting dose to study in humans.
Phase I and Phase II clinical trials
are often combined as one trial in rare disease research. Phase I trials typically involve between 10-50 people with the goal of making sure a therapeutic is safe. Phase II trials typically involve a few hundred people to confirm the safety of the therapeutic, including the potential to test different doses, and determine how effective a therapy is for a particular condition.
Phase III clinical trials
usually include hundreds to thousands of people and are designed to clearly show that a therapeutic is effective.
Phase IV clinical trials
are considered “post-market” research after a therapy is launched. You can think of these as long-term monitoring to track any safety issues, benefits, and overall clinical utility. This monitoring period may introduce new questions that scientists will need to investigate using basic science research.
Watch Dr. Rushing's December 2023 Presentation of the Research Roadmap here:
Watch an April 2024 Research Roadmap Update here:
