Science Snapshot - The Basics of Clinical Trials
Author: Tierney Baum, PhD, CSNK2A1 Foundation Strategic R&D Consultant
Edited by: Gabrielle Rushing, PhD, CSNK2A1 Foundation Chief Scientific Officer
A clinical trial is a lengthy process of testing out new treatments or devices to see how safe and effective they are in humans. They follow strict protocols and are conducted in phases, starting with small groups assessing safety and expanding to larger populations to determine how well the treatment works.
All drugs and medical treatments that we use have been through the rigor of clinical trials so they could eventually become approved by the Food and Drug Administration (FDA) to be used on patients for specific purposes (e.g., to treat a specific symptom or disorder). Before treatments become approved, there is a long path starting in non-human or ‘preclinical’ models; if these studies are successful, then they can move on to the multiple stages of clinical trials. In this Science Snapshot we will be breaking down these steps so you can understand how a treatment goes from an idea to reality.
Preclinical Studies
Preclinical studies are research experiments conducted in laboratories to test the safety, effectiveness, and biological activity of new drugs or treatments before they are tested on humans. These studies help scientists understand potential risks and benefits, guiding the development of therapies for human clinical trials. Before a treatment is ever considered to be used in a human it needs to be tested in animal models. These studies are most often designed using mice, which helps us understand their in vivo effects, or in vitro using human cells to help us understand biological effects.
In vivo – a process that takes places inside a living organism
In vitro – a process that takes place outside a living organism in a test tube, culture dish, etc.
These studies often help researchers understand how a treatment works rather than just its safety and overall effects. If there are favorable results in these studies, researchers can submit an
Investigational New Drug (IND) application to the FDA to request permission to conduct clinical trials.
Clinical Trial Stages
This outline describes the process for a standard clinical trial process. A future science snapshot will address clinical trials for rare disorders.
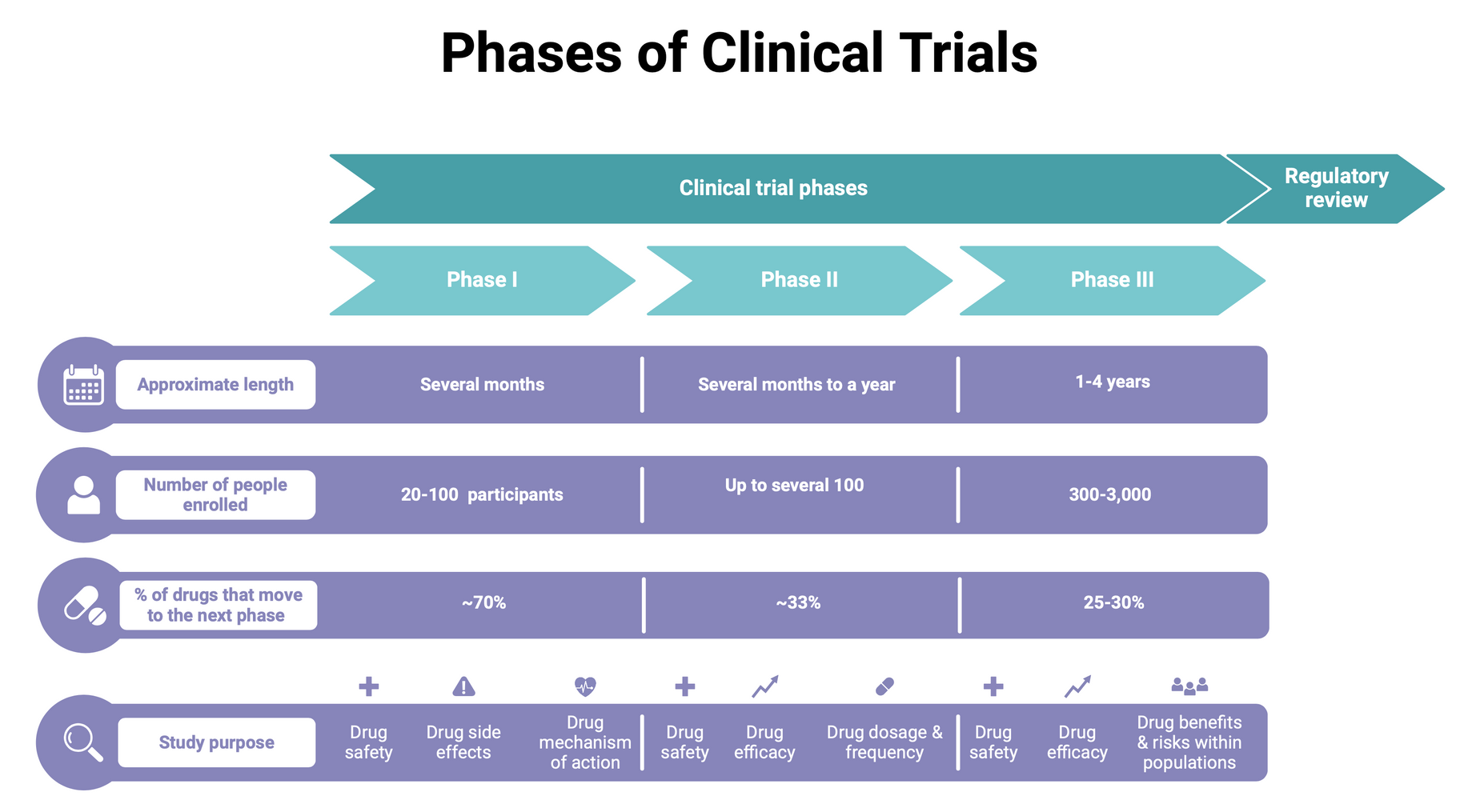
- Phase I Trial – drug or treatment is tested in a small group (~20-80 people) for the first time. The purpose is to study the drug or treatment to learn about its safety and identify any side effects.
- Usually last several months; 70% chance of moving on to Phase II
- Phase II Trial – drug or treatment given to a larger group of people (~100 – 300 people) to further understand its safety and effectiveness.
- Usually last several months to 2 years; 33% chance of moving on to Phase III
- Phase III Trial – drug or treatment given to large group of people (~1000-3000 people) to further confirm its effectiveness, monitor side effects, and compare to other current treatments.
- Usually last 1-4 years; 25-30% chance of moving on to FDA approval
Clinical Trial Design
To ensure a clinical trial is unbiased and effective, a lot of time is spent on study design. Bias in a clinical trial happens when the study is designed or conducted in a way that unfairly favors one outcome over another. This can make the results misleading and could put patients at risk. Unbiased means being fair and impartial, without letting personal opinions, feelings, or preferences influence decisions or outcomes. It involves evaluating facts and evidence objectively, ensuring that judgments or actions are not swayed by prejudice or preconceived notions.
For example, if a trial only includes certain types of people, like those who are healthier or younger, the results might not apply to everyone. Similarly, if researchers know who is getting the treatment and who isn’t, they might (even unintentionally) influence the results based on their expectations.
The following terms outline some essential parts of unbiased study design:
Placebo – an inactive treatment that resembles the test treatment (sugar pills, saline injection, etc.). It can be the fastest and most reliable way to show a new treatment’s effectiveness.
Randomization - the process by which treatments are assigned to a patient group by chance or randomly. This helps avoid bias in selecting which patients receive a specific treatment.
Blinding (or masking) – a study designed such that either researchers and/or participants are not aware of the specific treatment that the participants are receiving. This helps avoid bias during the collection of scientific data, ensuring it is accurate and not influenced by the patients or research team. When both researchers and participants are unaware it is called ‘double-blinded’.
Inclusion/Exclusion Criteria - metrics that help determine if a patient is suitable for a study. These may include age, biological sex, stage of disease, treatment history, medications, and other medical conditions.
Study protocol – the study plan outlining the following:
- Who qualifies
- How long the study will last
- How many people will participate
- What type of controls exist to limit bias
- How the drug is given and at what dose
- What assessments will be given
- What type of data will be collected and when
- How the data is reviewed and analyzed
- Which measure is considered the primary outcome measure*
- What type of compensation (if any) that participants will receive
- What plans are in place if something goes wrong
*The choice of outcome measure in a clinical trial is important. The primary outcome measure in a clinical trial is the main result that researchers focus on to determine if the treatment being studied is effective. It’s a specific, clearly defined goal that helps evaluate how well the treatment works. The primary outcome measure is chosen before the trial begins, during the planning phase, to ensure the study is focused and unbiased. Researchers select it carefully based on what is most important to understand about the treatment and its potential impact on patients.
For example, in a trial for a new cancer drug, the primary outcome might be whether the drug increases survival rates or reduces tumor size. This measure is important because it drives the entire study design, including how many participants are needed and how long the trial will last. A well-chosen primary outcome ensures the study answers the most important question about the treatment, providing clear and reliable information for doctors, patients, and regulatory agencies (e.g., FDA).
FDA Approval
Once a clinical trial is concluded, researchers will examine the data collected and decide whether the drug should move forward. If a treatment has proceeded through all stages with positive results and low risk to patients, they can submit a New Drug Application (NDA) to the FDA.
An unbiased team of experts reviews the data from the trials and determines if the study evidence shows that the drug is safe and effective. In these reviews the committee will often weigh risks against benefits, as well as the current available treatments and how this treatment improves options for the greater patient community. For example, if no other treatment options exist or if the disease is life-threatening, the FDA may be more inclined to approve the treatment. From start to possible approval, clinical trials often take around 6 years to complete. The overall success rate for clinical trials is low, with only 7.9% of trials reaching FDA approval. This means that over 90% of clinical trials fail, which represents a large financial burden and risk for pharmaceutical companies. Stay tuned for our next Science Snapshot focused on rare disease clinical trials!
Reference used for graphic:
FDA. Step 3: Clinical Research. U.S. Food and Drug Administration. Published January 4, 2018. https://www.fda.gov/patients/drug-development-process/step-3-clinical-research
